How To Use An Ambu Bag
OVERVIEW
- Bag-Valve-Mask (BVM) apparatus are also known as manual resuscitators and every bit self-inflating resuscitation systems
- examples include LaerdalTM, AmbuTM, HsinerTM, MayoTM, and Air VivaTM
USES
- assistants of high catamenia O2
- provision of PEEP (positive cease-expiratory pressure level)
- provision of controlled ventilation
- provision of augmentation of spontaneous ventilation
Description
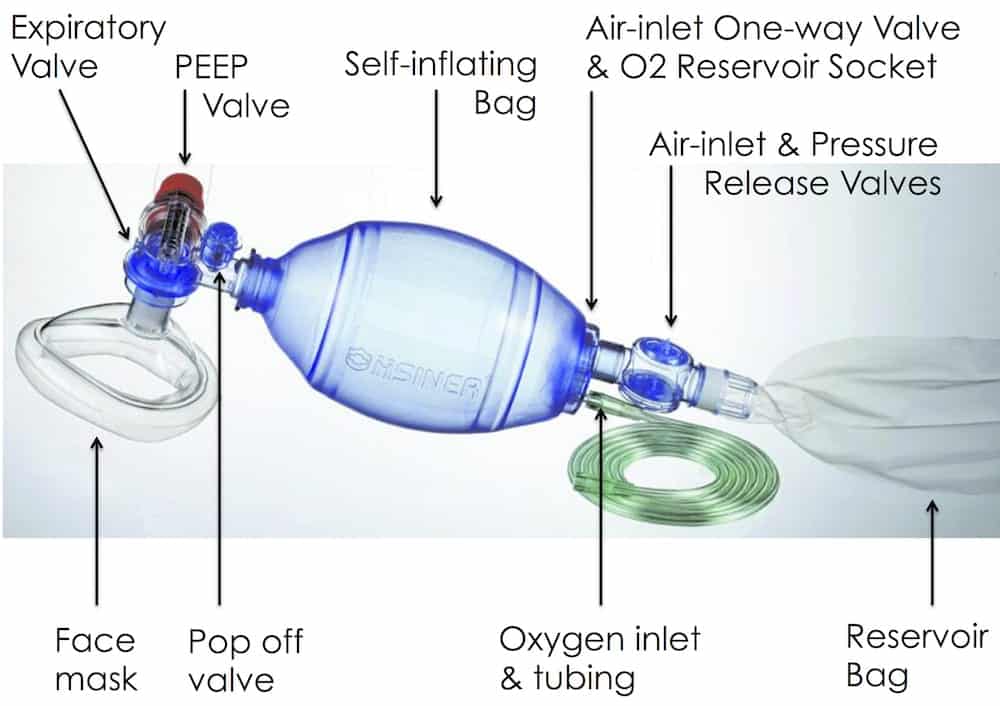
- self-inflating resuscitation device
- bag made of plastic materials that re-expand after being manually collapsed
- various sizes e.chiliad. Laerdal 240 mL, 500 mL, 1600 mL purse sizes for infants, children and adults
- oxygen inlet nipple
- air intake valve
- oxygen reservoir with 2 1 way valves
- reservoir is at least the volume of the bag
- oxygen flow rate equal to, or college than, the minute book of the patient allows 100% oxygen to exist delivered
- inlet valve allows room air to enter if fresh gas flow is inadequate and an outlet valve allow oxygen to catamenia out if pressure is excessive
- non-rebreathing valve that directs fresh flow of oxygen to the patient and prevents exhaled gas re-inbound the pocketbook
- standard xv mm adapter for attaching to masks or tubes
- able to adhere PEEP valve to exhalation port (either "congenital in" or detachable)
- can hold downwardly pop off valve (releases at nearly 60 cmH2O) to requite increased pressure level in the circuit
- Masks come in a range of sizes and designs
- opaque or clear plastic
- firm or air inflated cushion
- mouldings vary simply are designed to minimise dead infinite and fit
- some have specific names (due east.yard. Rendall Bakery Mask for paediatrics)
METHOD OF INSERTION AND/OR Apply
- Loftier period oxygen (e.g. 15 L/min) is attached to the system and it is attached to a mask or tube
- appropriate mask size
- place over mouth and olfactory organ
- tight fit
- open up airway using two-handed thumbs downward technique (with an banana bagging) in preference to the less effective one-handed C-E grip to ensure airway patency (best if OPA and NPAs in situ also)
- the bag is used to deliver oxygen to a spontaneously breathing patient or the bag compressed to manually ventilate them via a mask or tube (an assistant tin can provide ventilations)
Remember JAWS for the ii-handed two-thumbs downwards two person technique:
- Jaw thrust
- Airways (oral/nasal)
- Work together
- Slow, small clasp — half-dozen-7 cc/kg, over one-ii seconds, at <12/min, using low force per unit area.
COMPLICATIONS
- easy to hyperventilate patients and express ability to approximate tidal volumes
- unable to approximate lung compliance (cf. a ventilator or Water'south circuit)
- poor seal is common if 1-handed CE grip is used
- gastric distension
- aspiration
- claustrophobia
- exhaled secretions and moisture tin can event in exhalation valve dysfunction and increased resistance to expiration
- run a risk of barotrauma if pop off valve close equally unable to feel lung compliance with self-inflating bags
- if high costless gas flows are not used loftier FiO2 will not exist achieved
- equipment failure (east.g. due to incorrect assembly)
OTHER INFORMATION
Spontaneous ventilation
- Adminstered FiO2 during spontaneous ventilation tin can vary profoundly between devices
- Laerdal: FiO2 0.96
- Hsiner: FiO2 0.75
- Mayo: FiO2 0.55
- sufficient negative inspiratory pressure is required to overcome the patient inspiratory valve, otherwise, air will exist entrained instead of oxygen
- some duckbill valves are difficult to overcome when spontaneously breathing
- patients with reduced respiratory effort are particularly at risk
- As a safeguard in spontaneously breathing patients it is useful to coordinate 'assist' positive force per unit area ventilation with the patient'southward spontaneous efforts to ensure that the patient inspiratory valve is opening
Edentulous patients
- If the patient is edentulous, then suit the position of the mask like so:

Fom Racine SX, et al (2010), prototype from EM Updates (click image for source)
Alternatives to BVM
- use a ventilator to provide non-invasive ventilation
- employ of a Mapleson C (Waters circuit)
- in paediatrics, use of Mapleson E (Jackson-Ress modification of the Ayre's T-pieces)
VIDEOS
References and Links
Journal articles
- El-Orbany M, Woehlck HJ. Difficult mask ventilation. Anesth Analg. 2009 Dec;109(six):1870-fourscore. PMID: 19923516
- Gerstein NS, Carey MC, Braude DA, Tawil I, Petersen TR, Deriy L, Anderson MS. Efficacy of facemask ventilation techniques in novice providers. J Clin Anesth. 2013 May;25(3):193-7. PMID: 23523573.
- Hart D, Reardon R, Ward C, Miner J. Face up mask ventilation: a comparison of three techniques. J Emerg Med. 2013 May;44(five):1028-33. PMID: 23473817.
- Joffe AM, Hetzel S, Liew EC. A 2-handed jaw-thrust technique is superior to the one-handed "EC-clench" technique for mask ventilation in the apneic unconscious person. Anesthesiology. 2010 Oct;113(4):873-ix. PMID: 20808210.
- Khoury A, Hugonnot Due south, Cossus J, et al. From mouth-to-mouth to bag-valve-mask ventilation: development and characteristics of bodily devices – a review of the literature. Biomed Res Int. 2014;2014:762053. [article]
- Racine SX, et al (2010). Face up mask ventilation in edentulous patients: a comparison of mandibular groove and lower lip placement. Anesthesiology, 112 (5), 1190-three PMID: 20395823
Cream and web resources
- AirwayCam — Face Mask Ventilation
- EMCRIT — Wee – What the heck is a Mapleson B Circuit and Why You Probably Shouldn't Care (2014)
- Resus.ME — Thenar Eminence Based Medicine

Chris Nickson
Chris is an Intensivist and ECMO specialist at the Alfred ICU in Melbourne. He is also a Clinical Offshoot Acquaintance Professor at Monash University. He is a co-founder of the Australia and New Zealand Clinician Educator Network (ANZCEN) and is the Lead for the ANZCEN Clinician Educator Incubator program. He is on the Board of Directors for the Intensive Care Foundation and is a Starting time Office Examiner for the College of Intensive Care Medicine. He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical functioning of individuals and collectives.
After finishing his medical degree at the University of Auckland, he continued postal service-graduate training in New Zealand every bit well equally Australia'southward Northern Territory, Perth and Melbourne. He has completed fellowship training in both intensive care medicine and emergency medicine, as well as post-graduate preparation in biochemistry, clinical toxicology, clinical epidemiology, and health professional educational activity.
He is actively involved in in using translational simulation to improve patient care and the design of processes and systems at Alfred Health. He coordinates the Alfred ICU's education and simulation programmes and runs the unit's pedagogy website, INTENSIVE. He created the 'Critically Sick Airway' form and teaches on numerous courses around the world. He is one of the founders of the FOAM movement (Costless Open up-Access Medical teaching) and is co-creator of litfl.com, the RAGE podcast, the Resuscitology course, and the SMACC conference.
His one bully achievement is existence the male parent of iii amazing children.
On Twitter, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
How To Use An Ambu Bag,
Source: https://litfl.com/bag-valve-mask-bvm-ventilation/
Posted by: goldmanhocush64.blogspot.com


0 Response to "How To Use An Ambu Bag"
Post a Comment